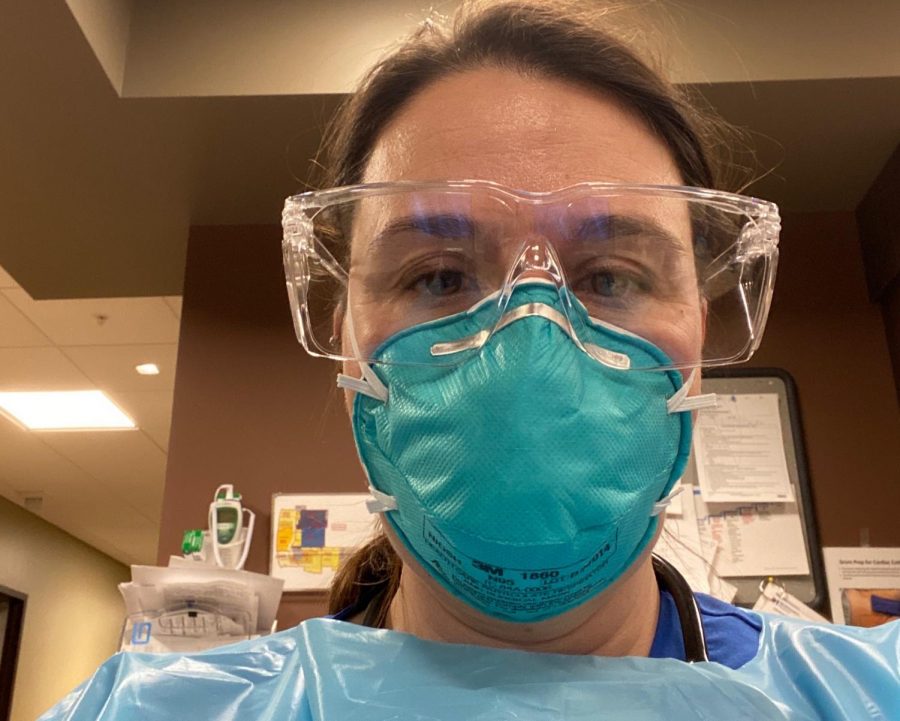
Provided by Jennifer Urbanczyk
Nurse Jennifer Urbanczyk.
…to be a nurse during the COVID-19 pandemic
I have not hugged my husband or children in literally over a month. I stay in the back bedroom and bathroom, away from my family. If I do need to come out of my room, I cover my face, stay more than 6 feet away from my family, and try not to talk while I am out, so as not to put aerosolized particles into the air. When I come out of my room, my family runs away.
Work has become more difficult. I work in the float pool of the hospital so I do not have a specific unit that I work in. I “float” to units that need extra help. Instead of just being the registered nurse, I am also the PCT (patient care technician or nurse’s aid), physical and occupational therapist, speech therapist, food service aid, and more. Only the nurses and physicians are allowed into the patient rooms.
We have many COVID patients in the hospital. One entire unit is devoted to only COVID patients and another is being equipped, should we need to open it. All hospital workers are now entering through one door and staff is stationed at the entrance.
Our badge is scanned and we answer questions. The questions are; does anyone that we live with have COVID?; are we feeling short of breath?; do we have a fever? If our answers are no, then we are given a sticker to place on our badge and one paper mask to use for the week.
Paper masks do not seal around the face. Air particles carrying germs can still get in and out and at times, it is difficult to get a good, deep breath in the mask. We take the masks off and place them into a paper bag to use for the remainder of the week.
The outside of the mask is considered dirty from all patients breathing and coughing. We have to be very careful not to contaminate ourselves when taking the masks off, putting them into the bags, and retrieving them for use again.
As per the CDC guidelines, we are only to use N95 masks if the patient is receiving an aerosol generating procedure, such as endotracheal intubations, airway suction or nebulizer treatments.
In order to preserve the PPE, physicians do not see the patient every day. Physicians rely on nurses’ abilities to assess the patient and communicate it to them so that the physician can put appropriate orders into the computer.
When it was believed that only China had COVID-19, no one could wear masks, as per the CDC guidelines, unless they, or a family member had been to China in the past 2 weeks.
Next, the CDC changed the guidelines and said that COVID-19 was airborne and that N95 masks should be worn only in the case of COVID-19 patients, and we wore them. Then, the CDC said that COVID-19 is transmitted by droplets and paper masks are sufficient. We are now wearing paper masks at all times while in the hospital.
We are caregivers so most of us are not worried about ourselves, but are concerned about bringing COVID-19 home to our families.
— Jennifer Urbanczyk
Most, if not all, of the physicians and staff are afraid. Curiously, I have heard of very few staff saying that they are afraid of getting COVID-19. We are caregivers so most of us are not worried about ourselves, but are concerned about bringing COVID-19 home to our families.